Africa: ‘No, Long Covid is Not a Thing in Your Head, You’re Sick’
Cape Town — allAfrica‘s Juanita Williams sat down with Professor Resia Pretorius, Stellenbosch University, who’s been researching how blood clots form and the impact of inflammation for two decades. Yesterday Pretorius delivered the keynote address at the 54th Mexican National Congress of Clinical Pathology in Puebla, Mexico, from October 30 to November 2, 2024.
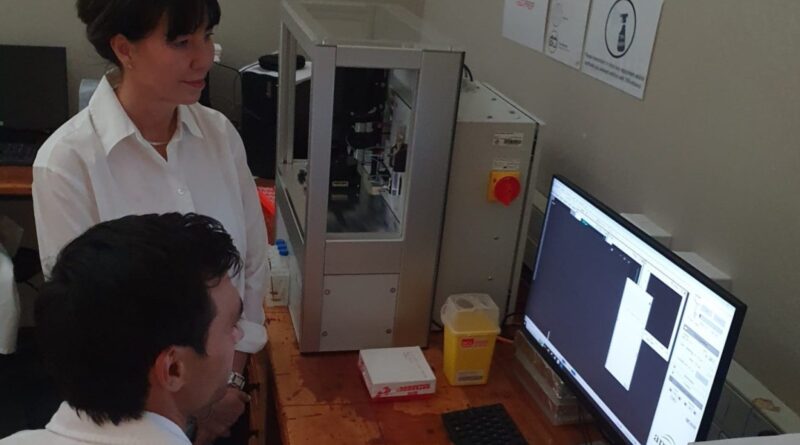
Pretorius has been at the forefront of acute Covid-19 and Long Covid research since 2022, when the professor and her team, first identified inflammatory microclots in blood samples from individuals who contracted Covid-19. Their symptoms persisted for months and, in some cases, even years.
“I’ve been working with my students to understand what molecules are in circulation in the blood that are caused by diseases,” Pretorius said. Her work researches conditions such as high blood pressure, cardiovascular disease, and diabetes, examining how these diseases elevate specific molecules in the bloodstream.
“If you look at diabetes, you will have too many glucose molecules in circulation inside your blood. We looked at those molecules and how they affect your blood, making it clot abnormally so that your blood becomes more viscous (sticky) and consequently increases your susceptibility to forming blood clots.”
Pretorius and her team focus on identifying the interactions between these molecules and plasma proteins, which can trigger abnormal blood clotting. She describes the normal clotting process: “For example, you cut yourself and you bleed, and you know that you don’t want to bleed forever; you need to form a little scab so that you can stop the bleeding and you can heal.”
Their symptoms persisted for months and, in some cases, even years
However, she said the dangers of abnormal clotting are caused by circulating inflammatory molecules. “You don’t want those molecules to interact with your blood that is soluble inside your body and then form small abnormal clots because inflammatory molecules have bound to the clots.”
Chronic inflammation due to, for example, cardiovascular disease, diabetes, and rheumatoid arthritis leads to an overload of inflammatory molecules, which can cause pathological clotting. Pretorius provides an example: “Many people will recognize that individuals with diabetes, for example, will get diabetic feet where the feet swell up and the legs are very sore. In some cases, someone with diabetes will get deep vein thrombosis, where they form a clot somewhere in the legs. Some people with diabetes can also die of a heart attack or stroke; they have a much higher propensity of dying than when you are healthy, so that’s all caused by pathological clotting.”
Pretorius’s work underscores the importance of understanding clotting pathology, particularly in the context of chronic inflammatory diseases. Her research aims to uncover the mechanisms behind abnormal clotting and develop strategies to mitigate the risks associated with these conditions. As the medical community continues to grapple with the complexities of clotting disorders, Pretorius’s contributions provide crucial insights into managing and potentially preventing life-threatening complications – particularly in the case of acute Covid-19 cases and what is now known as Long Covid.
It is not over
The 2023 Nature study, possibly the first statistical combination of results from separate studies “exploring prevalence, risk factors and symptomatology of long COVID in Africa”, included 25 studies, more than a thousand papers, and 29 213 patients.
Their findings, that almost half of the people studied exhibited Long Covid symptoms, and the most common reason they sought medical help was the most debilitating symptom – fatigue.
This is crucial information that points to the fact that the burden of Covid-19 in Africa and the world did not end with millions of deaths from this novel coronavirus.
It is not over.
African governments now face treating about 12 million citizens who recovered from the virus but may have ongoing symptoms such as persistent fatigue, shortness of breath, headaches, concentration difficulties, and muscle pain.
These symptoms often last for months and can severely impact daily functioning and quality of life (Nature). Many individuals are unable to work, leading to income loss and increased healthcare costs – straining the already overburdened healthcare systems in many countries.
And those statistics do not include people who have Covid-19 right now – acute cases or those without symptoms – and may later exhibit symptoms of Long Covid.
The Center for Disease in the U.S. defines Long Covid as “a serious illness that can result in chronic conditions requiring comprehensive care. Long Covid – also known as Post-Covid Conditions (PCC) long-haul Covid, Chronic Covid or Post-Acute Sequelae of SARS-CoV-2 infection (PASC) – can include a wide range of ongoing symptoms and conditions that can last weeks, months, or even years after Covid-19”.
Is there any information or guidance available for managing Long Covid symptoms, especially for individuals with pre-existing health conditions, like diabetes and high blood pressure?
My mother, who contracted Covid-19 in December 2020, initially seemed to recover but later experienced severe symptoms, including stomach issues and vomiting bile. Given her underlying health conditions, I wonder if there were any specific interventions or treatments that could have been considered during her repeated admissions to hospital in 2020 when post-Covid discussions were not as prevalent.
What resources or options are available for individuals dealing with lingering symptoms after recovering from Covid, especially for those with additional health concerns?
Unfortunately, whether it is 2020 or 2024, many individuals who contract Covid-19 still develop Long Covid. Unfortunately, developing effective treatments for various patient conditions can be a lengthy and challenging process.
Currently, a handful of clinicians who understand the disease will look at a patient and do a clinician-initiated treatment regime.
Now why? It’s that Long Covid and acute Covid-19 are new diseases.
So for clinicians to genuinely adapt to and have treatment regimes, they need to identify treatment options, and then it needs to go through clinical trials. We are a very, very, very long way from that! So unfortunately, what we have now is a selected handful of clinicians who fully understand the disease by not looking at it as a viral pneumonia, but looking at each patient in front of them.
You mentioned your mother suffered from TIA’s, which are transient ischaemic attacks, a mini-stroke. So clinicians wouldn’t have looked at treatment for that. They need to look at treatment of the symptoms because there’s no current treatment for Long Covid. The issue with Long Covid is there are over 200 different symptoms. It’s a syndrome, it’s not a single-origin symptom disease. So that’s what makes it difficult.
Unfortunately, it’s still very difficult.
Researchers, including myself and collaborators from prestigious institutions like Yale, Harvard, and Mount Sinai, are working diligently to understand these disease phenotypes (how the disease manifests in patients) and identify biomarkers (measurable indicators) to aid diagnosis.
We think it is a thrombophlebitis. While a big word, “thrombotic clotting,” simply refers to blood clots forming inside your blood vessels. This can be triggered by “endothelialitis,” which is inflammation of the lining of your blood vessels (VAs).
This inflammation can lead to problems throughout your body because it affects the health of your entire vascular system. It damages the inside of the blood vessels. It then prevents oxygen from travelling from your brain to your muscles to your heart adequately, and because you have an issue with oxygen transport, your vasculature doesn’t work well, and you’ve got immune dysregulation.
In some individuals, the virus may linger in the body even after recovering from the initial Covid-19 infection. This is called viral persistence. The virus might hide in various places, including inside the gut. Many people complain about gut dysbiosis or irregularities in the gut. Though they may not constantly feel unwell, some might experience vomiting. This is because the virus can significantly impact the gut. In some individuals, the virus goes and hides in the gut.
The inflammatory molecule that triggers the immune system, that triggers the blood clotting is then released slowly … into your body. It’s like a toxic little product being secreted by the virus that might be in hiding.
We think that Long Covid is immune-related. It’s clotting-related. While viral persistence might occur in some individuals, it doesn’t necessarily shape the constant release of inflammatory molecules in everyone.
What role does impaired blood flow, particularly due to conditions like atherosclerosis (the buildup of fats, cholesterol, and other substances in and on the artery walls) and mini-strokes, play in the development of vascular dementia, as observed in my mother’s case?

Sign up for free AllAfrica Newsletters
Get the latest in African news delivered straight to your inbox
Vascular dementia is a form of Alzheimer’s or Alzheimer’s type of dementia. It’s related to the vasculature not functioning properly in your brain. Vascular dementia can begin developing many years before a formal diagnosis is received. So the question is, whether perhaps the Covid event just fast-tracked it, that might be a possibility, we see that a lot.
Diabetes, high blood pressure, cholesterol, cardiovascular risk, all of those types of comorbidities in individuals… But it is in those individuals that we now know that acute Covid is much more severe. If we look at the Long Covid population, many of the people suffering from Long Covid will have had those types of comorbidities before their acute phase.
Now, we can also say that it might be just be that you become sicker faster. So that might have been the case with your mother. I’m not a clinician, so I can’t say anything about her specifically. But that’s what we see when we look at the patient groups.
Interestingly, many Long Covid patients also have never had comorbidities, they were quite healthy before they were in the acute phase. Some people also were perfectly healthy, and now struggle with things like Long Covid. That might be due to the genetics of the whole composition, perhaps they would have developed diabetes 10 years from now, before Covid. We simply don’t know what the trigger is, and why some who are perfectly healthy, develop Long Covid.
Could you clarify if the clinicians you mentioned earlier are specifically focused on treating Long Covid as a distinct condition?
I think it’s now well exhibited, there are hundreds of thousands of papers showing pathology (study of the condition).
Unfortunately, there are still individuals and clinicians who might think that it’s all in the patient’s head. They say they are just overthinking it, they (are) psychologizing it and they are gaslighting patients by saying: ‘You know what, just go and have a walk in the park, you will get over it.’
It is not that, it is not a thing in your head, you are sick.
Unfortunately, many people including clinicians might still be suggesting to some patients that there’s nothing to worry about. That it’s a psychological type of disease, because unfortunately, currently, the reason for it is that there are no real diagnoses for it.